Forget the so-called breastfeeding mommy wars.
The big issue isn’t whether well-educated, middle-class moms choose to breastfeed their babies.
The real problem – and one we should be talking fiercely about – is breastfeeding inequality.
Socio-economic forces are drastically affecting breastfeeding rates both in the US and globally. The result: huge numbers of mothers are NOT getting an equal opportunity to breastfeed their babies.
The stats may shock you.
In this article:
Breastfeeding Inequality [INFOGRAPHIC]
Related: The 15 Best Nursing Bras to Buy in 2021
Why it’s a problem
1) Socioeconomically disadvantaged moms are far less likely to breastfeed (or meet the American Academy of Pediatrics recommendations for optimal breastfeeding).
2) Babies born into conditions of hardship tend to receive less adequate healthcare, parental involvement, and nutritious supplementary solid food once weaning begins.
Essentially, the health benefits of breastfeeding are even more important for less-well-off mothers and their babies, and yet far fewer are breastfeeding.
This inequality is a shocking reality that must be tackled.

Related: The Best Nursing Pillows of 2021
Digging into the data
Let’s dig into the data to see the extent of the problem.
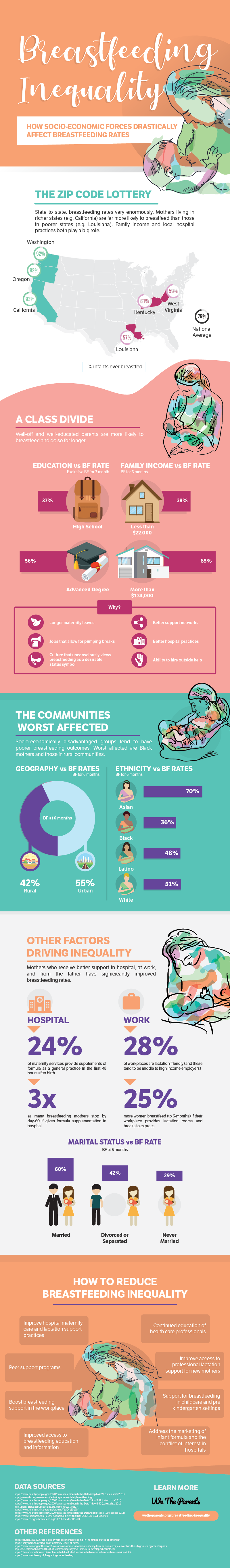
1) The zip code lottery
State to state, breastfeeding rates vary enormously. Mothers living in richer states, like California, are far more likely to breastfeed than those in poorer states, such as Louisiana.
Breastfeeding rates are correlated with family income and local hospital practices, among other factors. With regards to hospitals, 24% of babies born in the US are born in Baby-Friendly designated facilities.
The Baby-Friendly designation is awarded to hospitals that meet the Ten Steps to Successful Breastfeeding guidelines. These are a set of practices and procedures such as educating families to make informed decisions about infant feeding and offering expert lactation support throughout and beyond the hospital stay.
Currently, 1 in 6 hospitals or birthing centers in the US is Baby-Friendly designated. These are disproportionately represented in wealthier states where there is more money available to implement the initiative.
2) Education
The higher her level of education, the more likely a mother is to breastfeed her child. Only 36% of mothers whose education level is ‘high school’ exclusively breastfeed their babies for the first three months, while, in contrast, 56% of mothers with an advanced degree do so.
3) Earnings
38% of mothers living below the poverty threshold will breastfeed their baby until 6 months, whereas 68% of mothers from wealthy families (earning 6 times over the threshold) will do so.
This is a huge disparity, made all the more stark when you consider that, in 2016, there were 40.6 million people in poverty in the US. That’s a lot of babies not being breastfed simply because of the socioeconomic conditions they were born into.1Income and Poverty in the United States: 2016
census.gov
Some reasons that well-off mothers have improved breastfeeding rates are:
- Longer maternity leaves
- Jobs that allow for pumping breaks
- Better support networks
- Better hospital practices
- Ability to hire outside help
- A culture that unconsciously views breastfeeding as a desirable status symbol. (Source)
4) Urban/rural divide
Mothers in rural communities are less likely to breastfeed (42% of ‘rural’ mothers will breastfeed to 6-months, as opposed to 55% of ‘urban’ mothers).
Studies indicate that, rather than being caused by some inherent urban or rural culture, it has far more to do with confounding factors such as maternal ethnicity and poverty level.
Mothers living in rural communities are more likely to have a lower income and work in a job that doesn’t allow maternity leave or provide a lactation programme. They are also less likely to receive social breastfeeding support.2Rural-urban differences in breastfeeding initiation in the United States
ncbi.nlm.nih.gov
Related: 10 Best Nursing Covers for Breastfeeding (2021 Reviews)
5) Ethnicity
There are significant disparities in breastfeeding rates among Asian, Black, Hispanic, and White mothers. A major part of this trend has to do with socioeconomic measures such as poverty, education, and relationship status.3Breastfeeding gaps between white, black, and Hispanic mothers in the US
sciencedaily.com
Reasons for these differences, however, run deeper than just income. Other influencing factors include whether a mother receives supplementary breastmilk in hospital, whether she has experienced a close family member breastfeeding, or whether she believes that “breast is best”.
One startling statistic is that black mothers are nine times more likely to be given formula in the hospital than white mothers.
Another interesting insight is that Hispanic mothers from low-income families are more likely to breastfeed than their Black or White counterparts. The reasons appear to be that Hispanic mothers tend to experience another family member breastfeeding.
This intergenerational influence plays a huge role in whether a mother chooses to and successfully breastfeeds.4Racial and Ethnic Differences in Breastfeeding
pediatrics.aappublications.org
6) Formula use in hospital
Breastfeeding rates differ from hospital to hospital. It is in part a worrying reflection on the differing quality of maternity and lactation support. (The silver lining is that this area may be one of the easier ‘wins’ in the fight to reduce inequality.)
The use of formula milk within hospitals is an issue. Firstly, 66% of hospitals reported giving breastfeeding mothers free infant formula in their hospital discharge packs.
Hospitals generally do this as part of an agreement with commercial formula brands in return for free formula provision.
Perhaps even more worrying is that 24% of maternity services provide supplements of commercial infant formula as a general practice within the first 48 hours after birth.5Breastfeeding and the Use of Human Milk
pediatrics.aappublications.org
Both practices have been shown to negatively affect whether, and for how long, a mother exclusively breastfeeds.6Breastfeeding and the Use of Human Milk
pediatrics.aappublications.org
7) Lactation support in the workplace
In the US, only 28% of workplaces are lactation friendly (ie, provide comfortable and private rooms where mothers can use breast pumps and store milk safely). These tend to be in middle to high-income jobs.
This is bad news for the majority of working mothers and creates another dimension of inequality. Especially since 25% more women breastfeed to 6-months if their workplace provides decent lactation rooms and breaks to express. 7Why invest, and what it will take to improve breastfeeding practices?
thelancet.com
Clearly, there’s a long way to go before mothers are properly supported in their breastfeeding efforts within the workplace. This has a significant impact on the number of babies being breastfed across the US.
8) Marital status
Married women are more than twice as likely to breastfeed for 6-months than unmarried mothers. Clearly, the support a father can provide plays a significant role.
New Zealand researchers found that when dads cooked dinner (and washed up), it had a positive effect on the mother’s breastfeeding success. It allowed mom time to focus on feeding the baby and provided her with the rest that helped maintain her milk supply.8Partners who do this one (simple) thing can improve moms’ breastfeeding rates
mother.ly

Related: Best Nursing Tank Tops of 2021 (Tried, Tested, and Affordable)
How to reduce breastfeeding inequality
Too few mothers follow the AAP’s optimal breastfeeding recommendations. Were this a result of well-educated, well-informed, and well-off women choosing alternative nutrition options, that would be one thing.
Unfortunately, in reality, many babies are formula-fed because their mothers are not aware of the possible health risks or simply don’t have the practical support needed (at work or home) to make breastfeeding optional.
This is unfair and impacts the health of thousands of US mothers and babies each year. It has been estimated that annual excess deaths attributable to suboptimal breastfeeding total 3,340, 78% (2605) maternal and 22% (735) infant.9Suboptimal breastfeeding in the United States: Maternal and pediatric health outcomes and costs
ncbi.nlm.nih.gov
So how can we reduce breastfeeding inequality?
While there is no easy fix, there are several strategies that have been highlighted and could use public awareness and support. These are:
- Maternity/lactation support – Improve hospital maternity care and lactation support practices. For example, increasing the number of Baby-Friendly Designated hospitals across the US, especially in states with more poverty.
- Educate professionals – Continued education of healthcare professionals, such as doctors, nurses, midwives, and lactation consultants, to improve their knowledge, skills, attitudes, and behaviors toward breastfeeding support.
- Improve new mother access to professional lactation support – This can be done in different ways, such as in-person, online, telephone, or group. It can involve home visits or breastfeeding clinics within the community.
- Peer support programs – Peer support is a powerful mechanism for helping mothers reach their breastfeeding goals. Effective peer support typically requires leaders to be trained as facilitators. Mothers then share emotional support as well as guidance and problem-solving advice, eg, tips for getting a good latch or breastfeeding in public.
- Boost breastfeeding support in the workplace – There are numerous ways in which employers can support mothers to continue breastfeeding. These include developing corporate policies, and providing adequate lactation spaces and equipment, while allowing women the flexibility to use them. Onsite child-care and allowing babies at the workplace also helps.
- Support for breastfeeding in childcare and pre-kindergarten settings – Many mothers have older siblings attending early care education centers (eg, Head Start or pre-K). This solution involves improving the support that these centers give to breastfeeding mothers, eg, welcoming breastfeeding mothers to come into the center, or training staff to handle the storage and use of pumped breastmilk.
- Improved access to breastfeeding education and information – While many mothers have heard the message that “breast is best”, many new mothers do not have direct experience of breastfeeding. It is vital that breastfeeding education and information is introduced into all communities, especially minority groups that can be harder to reach.
- Address the marketing of infant formula and the associated conflict of interest in hospitals – There exist well-established links between commercial formula companies and hospitals. In return for free infant formula for babies that need it, many hospitals agree to give away free formula with discharge bags. There is also a high incidence of hospitals routinely supplementing breastfed infants with formula within the first 48-hours. Both these practices lead to an increased uptake in formula use and a corresponding drop in breastfeeding rates. It’s important that marketing practices designed to reduce breastfeeding rates are dismantled and replaced with those that don’t involve a conflict of interest.

Related: Itchy Breasts While Nursing (what, why, and how to fix it)
Equality of knowledge and breastfeeding opportunity
The breastfeeding mommy war is a huge distraction from the real problem of inequality. If a well-informed mother makes a carefully considered decision not to breastfeed, that is entirely up to her. This isn’t the issue.
The actual issue is that not all mothers have equal knowledge or opportunity when making the right breastfeeding choice for themselves and their babies.
If breastfeeding inequality is tackled, then hundreds and thousands more babies will be breastfed. This, in turn, will lead to the improved health of mothers and babies and economic benefits to society.
Let’s shift the focus of the conversation to breastfeeding inequality. It’s here that some major victories in health and wellbeing can be made.
What do you think?
Please feel free to share your thoughts and opinions. We’d love to hear from you in the comments below.